If you’ve ever felt suddenly dizzy, lightheaded, or even faint while on the toilet, you know how unsettling the experience can be. One moment you are fine, and the next, a wave of strange sensations washes over you, leaving you feeling scared and confused. Please know you are not alone in this. This experience, while startling, is your body’s way of communicating through a powerful mechanism known as the vagal response.
This response involves the vagus nerve, a sort of information superhighway that connects your brain to your gut and other vital organs. Instead of being a sign that something is terribly wrong, it’s often a signal that your nervous system is feeling sensitive or overwhelmed. Let’s gently explore what happens during a vagal response, why it can occur during a bowel movement, and how you can learn to listen to its message with compassion rather than fear.
Understanding the Vagal Response During a Bowel Movement
This experience, while unsettling, is your body’s way of communicating. It involves the vagus nerve, your body’s information superhighway. Let’s gently explore what happens and why it’s a gut-brain signal.
What Is a Vagal Response? A Simple, Gentle Explanation
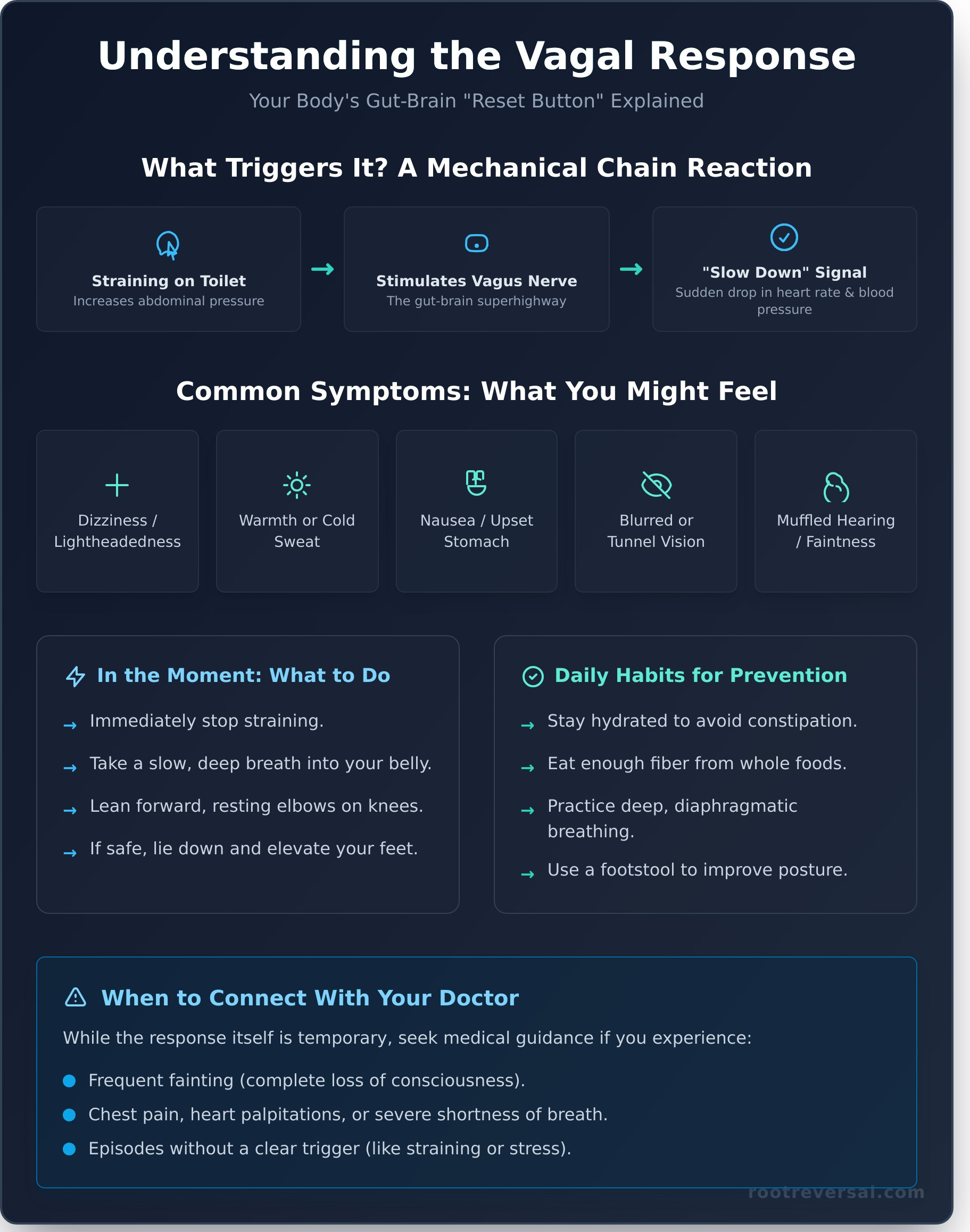
Think of a vagal response as your body’s powerful, automatic reset button. The vagus nerve is a key part of the parasympathetic nervous system, which is responsible for your body’s “rest and digest” functions. When this nerve is overstimulated, it can trigger a sudden, temporary drop in your heart rate and blood pressure. This is a natural reflex designed to calm your system down, but the rapid shift is what causes those alarming symptoms. It’s a physiological process, not necessarily a sign of an underlying disease.
Why Does It Happen on the Toilet?
The connection to bowel movements is purely mechanical. When you strain on the toilet, you increase the pressure inside your abdomen. This pressure can physically stimulate the vagus nerve as it passes through your chest and stomach. For a nervous system that is already sensitive or on high alert, this physical trigger is enough to overstimulate the nerve, causing it to send a strong “slow down” signal to your heart and blood vessels. It’s a physical act that gets amplified by the current state of your nervous system.
Common Symptoms: Validating Your Experience
It’s important to validate what you feel, as these sensations are very real. A vagal response can bring on a cluster of symptoms quite suddenly. You might experience:
- A sudden feeling of lightheadedness or intense dizziness.
- A wave of warmth spreading through your body, or breaking out in a cold sweat.
- An abrupt sense of nausea or an upset stomach.
- Changes in your vision, like seeing spots, tunnel vision, or blurred sight.
- Muffled hearing or a ringing in your ears, coupled with a feeling of faintness.
From Frightening Symptom to Body Signal: A New Perspective
It is completely natural to feel frightened when your body behaves in such an unpredictable way. But we can gently re-frame this experience. Instead of viewing it as a terrifying symptom, consider it a powerful signal. A vagal response is often a sign of a sensitive, dysregulated nervous system that is trying to get your attention. It’s an invitation to pause, breathe, and listen more closely to what your body truly needs.
Is a Vagal Response Dangerous?
For the vast majority of people, the vagal response itself is temporary and not life-threatening. The episode usually resolves within a minute or two once the trigger is removed. The primary danger comes from the potential for injury if you faint and fall. The experience is a signal that your system is out of balance, but it is not the root problem itself. Learning to recognize the early warning signs is the key to keeping yourself safe.
When to Connect With Your Doctor
While most vagal responses are benign, it is always wise to seek medical guidance to rule out other conditions, especially if your symptoms are new or severe. Please connect with your doctor if you experience any of the following:
- You frequently lose consciousness completely.
- The episode is accompanied by chest pain, significant shortness of breath, or heart palpitations.
- It happens without any clear trigger, such as straining or emotional distress.
The Link Between Anxiety, Stress, and Your Gut
Your nervous system is the soil in which your health grows. When you live with chronic stress or anxiety, your nervous system can become chronically dysregulated, making your vagus nerve far more sensitive to triggers. Anxiety often creates physical tension throughout the body, including in the pelvic floor and abdominal muscles, which can lead to straining without you even realizing it. This is a classic, tangible example of the gut-brain connection in action—your emotional state is directly influencing a physical reflex. Feeling overwhelmed by gut-brain symptoms? Discover our gentle approach.
Gentle Practices to Soothe Your System and Prevent Episodes
The beautiful truth is that you have the power to create more balance and resilience in your body. The goal is not to forcefully stop the symptom but to create a sense of safety from within. These are small, nurturing steps you can take to calm your entire system, making these episodes less likely to occur.
In the Moment: What to Do When You Feel It
The moment you feel that familiar wave of dizziness or warmth, respond with gentle action. First, immediately stop straining and take a slow, deep breath into your belly. If you are sitting, lean forward and rest your elbows on your knees, lowering your head. If possible and safe, the best course of action is to lie down on the floor and elevate your feet slightly until the feeling passes. Do not try to push through it.
Daily Habits for a Calmer Nervous System
Prevention begins with small, consistent acts of self-care. Ensure you are drinking enough water throughout the day and eating enough fiber from whole foods to help prevent constipation and the need for straining. Practice mindful, diaphragmatic breathing before and during your time on the toilet to keep your body relaxed. You might also consider placing a small stool under your feet to elevate your knees above your hips, which aligns your colon for easier elimination.
Addressing the Root Cause Holistically
True, lasting healing comes from addressing the underlying state of your nervous system. By learning techniques for nervous system regulation, you create a foundational sense of safety and resilience from within. This work helps your body move from a state of chronic “fight-or-flight” to one of “rest-and-digest,” where your vagus nerve can function in a more balanced way. A holistic coach can be an invaluable guide on this journey, helping you reconnect with your body’s innate wisdom.
Frequently Asked Questions
What is the difference between a vagal response and vasovagal syncope?
A vagal response refers to the range of symptoms caused by the stimulation of the vagus nerve (dizziness, nausea, sweating). Vasovagal syncope is the medical term for fainting that occurs as a result of that response. In other words, syncope is the end point of a severe vagal response.
Can anxiety alone cause a vagal response?
Yes. A strong emotional trigger, like intense fear, anxiety, or even the sight of blood, can be enough to overstimulate the vagus nerve and cause a full vagal response, sometimes leading to fainting. This is because your emotional state and your nervous system are deeply intertwined.
How can I stop straining during bowel movements naturally?
Focus on long-term gut health. Stay hydrated, gradually increase your intake of soluble fiber from sources like psyllium husk, oats, and fruits, and consider using a squatting stool. Most importantly, give yourself unhurried time on the toilet and practice deep belly breathing to relax your pelvic floor muscles.
Are certain foods or drinks known to trigger a vagal response?
While not a direct trigger, dehydration and low blood sugar can make you more susceptible to a vagal response. Large, heavy meals can also divert blood to your digestive system, which can contribute. The most direct connection, however, is the physical act of straining, often caused by a low-fiber diet and dehydration.
Is this related to IBS or other gut conditions?
Yes, there can be a strong connection. People with IBS often experience visceral hypersensitivity, meaning the nerves in their gut are extra sensitive. They may also struggle with constipation or diarrhea, leading to more straining or stress during bowel movements, which can increase the likelihood of a vagal response.
Your body is always communicating with you, and a vagal response is one of its most powerful messages. By meeting this experience with curiosity and compassion, you can transform fear into an opportunity for deeper healing. Addressing the root cause—a dysregulated nervous system—allows you to build a foundation of safety and trust within your own body. Ready to find the root of your gut-brain symptoms? Book a pre-consultation call today.